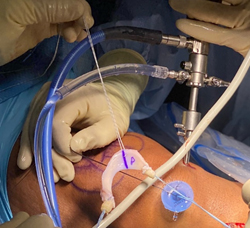
Shoulder Rotator Cuff Reconstruction
There are four rotator cuff muscles in the shoulder than attach to the humerus bone by way of a tendon. Each of the four rotator cuff muscles function to perform a specific motion to the shoulder allowing us to throw a ball or comb our hair. Trauma, repetitive impingement, and aging can lead to partial or complete rotator cuff tendon tears making normal shoulder activities difficult to perform. Rotator cuff tears that are large, retracted, and chronic may not be repairable back to their bone attachment site. Instead, a retracted rotator cuff tendon may be reconstructed by bridging an allograft between the bone and the retracted edge of the tendon using an arthroscopic technique. If the tendon can be repaired directly back to the bone, a graft can also be used to augment the repair to provide more collagen thickness to the repair and increase the pull-out strength of the sutures holding the tendon to bone - which can be useful in the setting of a degenerative tendon. To see if you are a candidate for a rotator cuff reconstruction or augmentation, contact your orthopedic surgeon.
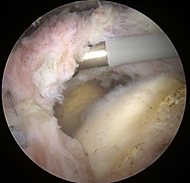
Before and after allograft augmentation and reconstruction of a rotator cuff tear.
Shoulder Superior Capsule Reconstruction
One or more of the four rotator cuff tendons may tear from their humerus attachment site. As the tear enlarges and retracts further away, the rotator cuff muscle belly may begin to atrophy from disuse and may eventually become replaced with fat (adipose) cells, which is an irreversible process. Without the normal coupling effect of intact rotator cuff tendons, the humeral head no longer remains stable and may subluxate superiorly eventually leading to shoulder joint arthritis. Patients often present with significant weakness, loss of shoulder range of motion, and persistent pain. In patients over the age of 70, a reverse total shoulder replacement may be recommended to restore function and reduce pain. However, in younger patients a reverse shoulder replacement may not be an ideal solution due to concerns of implant longevity. A significantly retracted rotator cuff tendon with atrophy of the muscle belly may not suitable for direct repair or reconstruction. Instead, a surgical reconstruction of the superior capsule may help keep the humerus from translating superiorly and therefore provide improved shoulder function and reduced pain. A graft, procured from the patient’s iliotibial band or from an allograft, is placed and secured into the shoulder joint using an arthroscopic technique. Clinical studies have validated this procedure to improve both function and pain. To see if you are a candidate for a superior capsule reconstruction, contact your orthopedic surgeon.
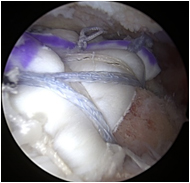
Images show before and after of a superior capsule reconstruction of the shoulder.
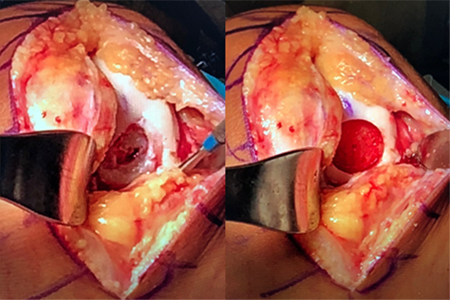
Hip Labrum (or Labral) Reconstruction
The hip labrum is a gasket-like cartilage structure that lines the acetabulum, or hip socket. Among its many important functions, the labrum helps to keep the hip stable and prevents the hip from developing arthritis. When patients present with extensive labrum tears or have large calcifications within the labrum, surgical repair of the labrum may not be possible. These patients may instead benefit from a surgical reconstruction of the labrum whereby a new labrum is created and grafted into the hip. A labrum reconstruction can be made from tissue procured from around the hip such as the iliotibial band or from allograft tissue. Using an arthroscopic technique through small key-hole incisions, the labrum can be sewn onto the acetabulum rim. The graft can be used both as an augment and placed next to the patient’s native labrum or to fill a labrum defect. Studies have shown that labrum reconstructions can successfully reduce patient-perceived pain and improve hip function. To see if you are a candidate for a hip labrum reconstruction, contact your orthopedic surgeon.

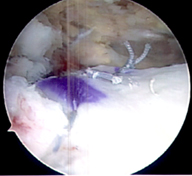
Hip labrum allograft reconstruction.
Knee Meniscus Transplantation
The meniscus is a fibrocartilage structure in the knee that helps disperse the contact forces between the femur and tibia bones. A meniscus tear may occur with a twisting or shear force applied to the knee. If the meniscus can be repaired, this may help restore normal kinematics of the knee joint. However, certain meniscus tears may not be repairable or may re-tear despite surgical repair. If the meniscus is partially or completely resected, this may result in knee pain and lead to the progression of osteoarthritis. A meniscus transplantation may be performed using allograft meniscus tissue which is placed and secured into the knee joint using arthroscopic-assisted techniques. Clinical results have shown excellent results in alleviating pain at the knee. To see if you are a candidate for meniscus transplantation, contact your orthopedic surgeon.
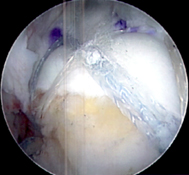
Meniscus allograft immediately before implantation.
Before graft implantation.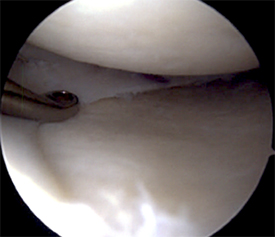
Meniscus allograft after implantation.
Knee MACI® (Matrix Induced Chondrocyte Implantation)
Matrix-induced autologous chondrocyte implantation, or MACI®, is a cartilage grafting procedure in which a patient's own cartilage cells are used to regrow new cartilage for the knee joint. The procedure therefore is a two-part procedure. The first procedure requires the harvest of approximately a tic-tac size piece of cartilage from the knee. This cartilage is then sent to a laboratory where the cells are grown and expanded. The cartilage cells are then placed onto a resorbable collagen membrane and are sent back to reimplantation. The membrane is then glued into the cartilage defect of the knee during a second procedure using either arthroscopic-assisted or open techniques, depending on the size and location of the cartilage lesion.
Extensive research has shown significant improvements in knee pain and function with MACI®. To see if you are a candidate for a MACI® procedure, contact your orthopedic surgeon.

MACI cartilage cells on a collagen membrane being grafted back into the knee. Fibrin glue is used to hold the graft in place.
Knee Osteochondral Allograft Transplantation
Full-thickness cartilage defects of the knee that also involve the deeper bone layer are called osteochondral lesions. Osteochondral lesions may be caused by osteochondritis dissecans or from traumatic events such as a twisting injury of the knee. Osteochondral lesions that are relatively small in size can be grafted with a procedure known as Osteochondral Autograft Transplantation Surgery, or OATS. A plug of cartilage and bone is harvested from another part of the knee and is then implanted into the defect. The size of the lesion dictates how many plugs need to be taken. Therefore, in larger or multiple lesions, an osteochondral allograft may be used in order to reduce the amount of cartilage taken from the patient’s own knee. These special allografts are sized-matched to fit the osteochondral defect. The surgeon first prepares the knee defect to accept the osteochondral graft. The osteochondral allograft is then prepared using special tools. The graft is then press-fit into the recipient site in the knee. The patient is allowed to resume weight bearing activities over the next few weeks and may return to functional activities over the ensuing months once the graft has fully incorporated. To see if you are a candidate for an osteochondral autograft or allograft procedure, contact your orthopedic surgeon.
Femoral condyle osteochondral lesion is prepared to receive the osteochondral allograft.

The osteochondral lesion allograft is prepared and implanted into the recipient site with a press-fit technique.
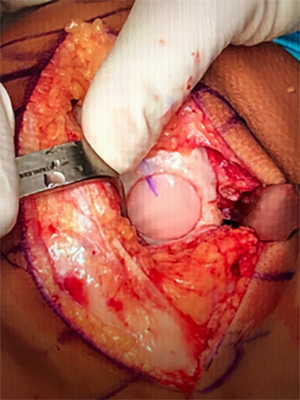
Osteochondral allograft implanted into the knee.